Press notes 01/02/2023
A collaborative management guide is being developed on the use of psychotropic drugs in mental health
Developed by a research team from the URV and the UOC, this tool was designed so that users of psychotropic drugs could have access to mechanisms of participation and take co-responsibility for their treatment
Developed by a research team from the URV and the UOC, this tool was designed so that users of psychotropic drugs could have access to mechanisms of participation and take co-responsibility for their treatment
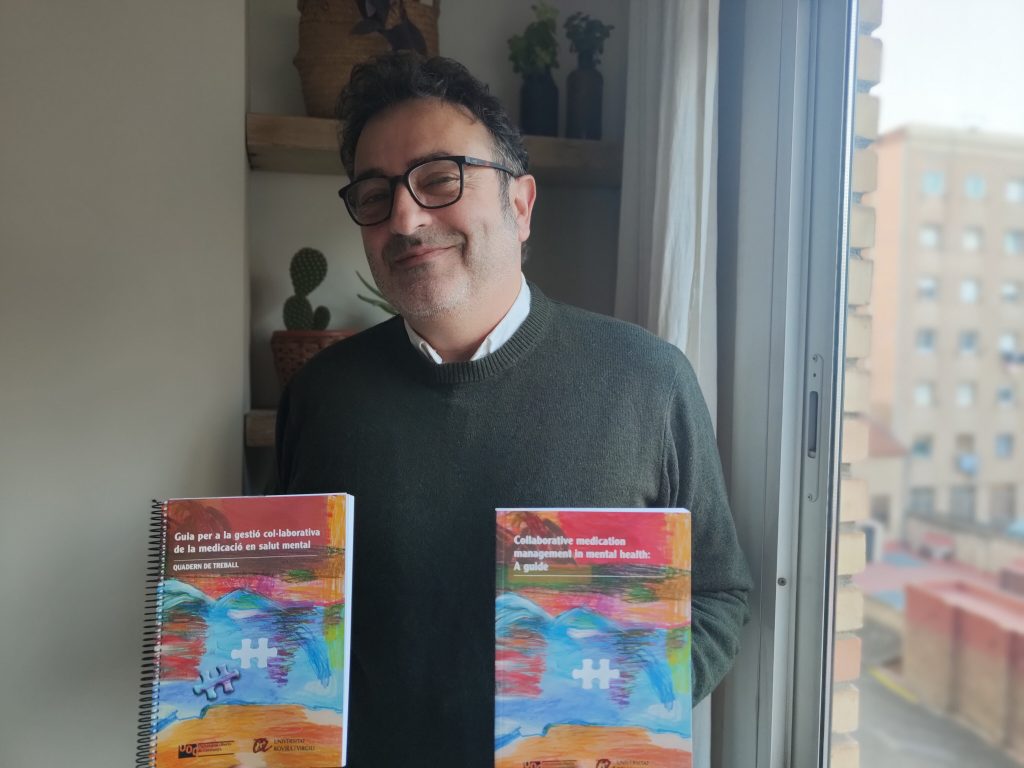
Antipsychotic medication is the primary treatment for mental disorders such as schizophrenia. However, between 25 and 50% of people diagnosed with this disease claim not to feel satisfied with the medication they usually take because it does not give them the result they expect, despite complying with it on a regular basis. This lack of satisfaction is due to the side effects and health risks of the medication, such as weight gain, the risk of metabolic syndrome or the effect on self-esteem. There are also social connotations associated with this type of drug, such as stigmatization or discrimination. Antipsychotics have also been shown to be useful in alleviating positive symptoms of psychosis, such as hallucinations and delusions, but do not work as well in addressing negative symptoms, such as apathy or loss of motivation. All these factors make it difficult to comply with the therapeutic alliance, understood as the collaborative bond between the patient and the therapist. Now, an investigation coordinated by the URV sheds light on the existence of other mechanisms by which users can take part in and take co-responsibility for their own treatment. As a result of this research, the Guide for the collaborative management of medication in mental health has been drawn up.
The result of work done by the URV’s research group MARC (Medical Anthropology Research Center) in collaboration with a research group from the UOC, this tool has been developed over more than three years. The aim of the study was to investigate the perceptions and subjective experiences associated with psychotropic drugs in Catalonia, especially antipsychotics, as well as their effects on the quality of life and the everyday life of consumers. The research aims to implement comprehensive and sustainable health policies within the field of mental health and was based on interviews, questionnaires and discussion groups with users of psychoactive drugs, carers and professionals. It is an ethnographic, qualitative and observational study, which does not involve any clinical or pharmacological procedures.
The result of work done by the URV’s research group MARC (Medical Anthropology Research Center) in collaboration with a research group from the UOC, this tool has been developed over more than three years. The aim of the study was to investigate the perceptions and subjective experiences associated with psychotropic drugs in Catalonia, especially antipsychotics, as well as their effects on the quality of life and the everyday life of consumers. The research aims to implement comprehensive and sustainable health policies within the field of mental health and was based on interviews, questionnaires and discussion groups with users of psychoactive drugs, carers and professionals. It is an ethnographic, qualitative and observational study, which does not involve any clinical or pharmacological procedures.
The guide is designed for people who have experienced mental suffering and have been prescribed psychotropic drugs as a therapeutic measure. It hopes to generate dialogue and debate about this type of treatment. It also aims to enhance the participation and decision-making capacity of the people who consume psychotropic drugs, especially antipsychotics, in order to facilitate access to all the necessary information about the drugs and their alternatives, since this type of consumer is generally at risk of exclusion and has limited personal autonomy. Created in co-authorship by researchers, mental health professionals, users and caregivers, the guide provides information about drugs and their side effects, experiences or short stories in the first person, and tools to create a work space in which medication and mental health can be discussed.
One of the main innovative aspects of the guide are the questions that the readers are asked, so that they can reflect and develop a personal opinion and position on medication. Some of them are “What do I feel when I feel bad?”, “How do I identify this feeling?” or “What are my favourite daily activities?”
From Canada to Brazil and, finally, Catalonia
Collaborative Medication Management (CCM) is an initiative that was developed in the early 1990s in Quebec by research teams in collaboration with civil society and, above all, users of mental health services and their advocacy groups. In recent years, it has been given an exponential boost as it has been moved to Brazil under the framework of L’Alliance Internationale de Recherche Universités – Communautés, Santé Mentale et Citoyenneté (ARUCI-SMC), where it has been put into practice in the public universities of the states of São Paulo, Rio Grande do Sul and Rio de Janeiro.
The project has now reached the URV, where an in-depth analysis of these GCM experiences has been made. Another study has been made of how medicines are managed in Catalonia in order to analyse the obstacles that exist in the collaborative management of medication and the spaces for the co-production of shared solutions between users, professionals and carers. Finally, this GCM guide has been published as a book, adapted to the social and cultural reality of Catalonia. These are not medication guides, but tools for users to use and reflect on a daily basis.
Continuity of research
The research findings pointed out three main obstacles to collaboration between participants (users, clinicians and family caregivers). First of all, they had different understandings of the concept of discomfort: the clinicians attributed it to the symptoms of the disorder and the users to the adverse effects of the medication. Secondly, there were differences in defining the awareness of the disorder. The professionals associated awareness of the disorder with treatment compliance, while caregivers associated it with self-care, and patients spoke of “awareness of suffering”, which encompassed discomfort in a broad sense and included the experience of marginalization and stigma, as well as the adverse effects of biomedical treatments.
Finally, discordant expectations about clinical communication were also highlighted. These can be summed up by the two meanings of the word “treatment”: one of the meanings is a relationship between two people and a recognition of the other as an individual; and the other is an intervention that is carried out more on an object (the disease) than on a subject (the patient). These obstacles facilitate coercive practices and the desubjectivation of patients, which are precisely those areas that the Guide aims to influence and generate autonomy, the empowerment of those affected, and clinical practices that involve shared decisions.
Various institutions have participated in the research: the Badalona II Adult Mental Health Center, the Nou Barris Adult Mental Health Center, the Catalan Mental Health Federation, La Muralla, the Aixec SCCL Cooperative, the Radio Nikosia Sociocultural Association, the Catalan Mental Health Congress Foundation (FCCSM) and the Saräu Inclusive Leisure Association.
The research team says that they will be able to continue with the project if they can provide a proof of concept – that is, prove that the concept or theory is viable – or carry out a clinical trial.
Reference: The collaborative management of antipsychotic medication and its obstacles: A qualitative study. Ángel Martínez-Hernáez, Asun Pié-Balaguer, Mercedes Serrano-Miquel, Nicolás Morales-Sáez, Andrea García-Santesmases, Deborah Bekele, Elisa Alegre-Agís. Social Science&Medicine. February 2020. DOI: https://doi.org/10.1016/j.socscimed.2020.112811
